Degenerative And Demyelinating Diseases Of The Nervous System
El Paso, TX. Chiropractor, Dr. Alexander Jimenez focuses on degenerative and demyelinating diseases of the nervous system, their symptoms, causes and treatment.
Table of Contents
Degenerative & Demyelinating Diseases
Motor Neuron Diseases
- Motor weakness without sensory changes
- Amyotrophic lateral sclerosis (ALS)
- ALS Variants
- Primary lateral sclerosis
- Progressive bulbar palsy
- Inherited conditions that cause anterior horn cell degeneration
- Werdnig-Hoffmann disease in infants
- Kugelberg-Welander disease in children and young adults
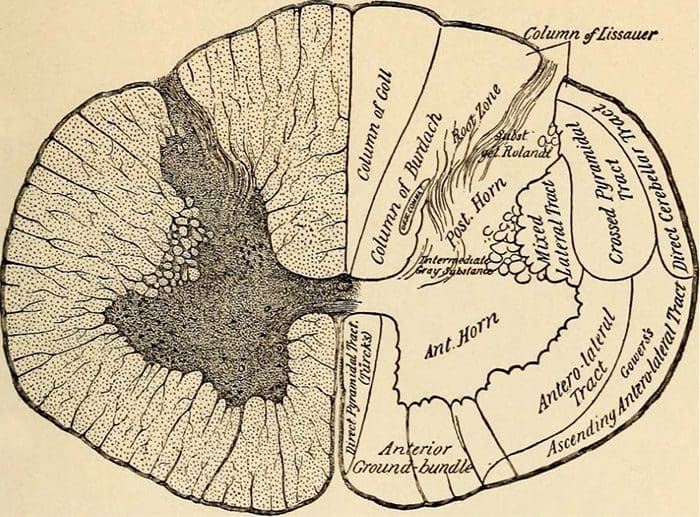
Amyotrophic Lateral Sclerosis (ALS)
- Affects patients 40-60 years of age
- Damage to:
- Anterior horn cells
- Cranial nerve motor nuclei
- Corticobulbar and corticospinal tracts
- Lower motor neuron findings (atrophy, fasciculations) AND upper motor neuron findings (spasticity, hyperreflexia)
- Survival ~three years
- Death results from weakness of the bulbar and respiratory musculature and resultant superimposed infection
ALS Variants
- Usually eventually evolve into typical ALS pattern
- Primary Lateral Sclerosis
- Upper motor neuron signs begin first, but patients do eventually have lower motor neuron signs as well
- Survival can be ten years or longer
- Progressive Bulbar Palsy
- Selectively involves the head and neck musculature
Inherited Motor Neuron Conditions
- Anterior horn cell degeneration
- Werdnig-Hoffmann disease
- Affects infants
- Kugelberg-Welander disease
- Affects children and young adults
 Church, Archibald. Nervous and Mental Diseases. W.B. Saunders Co., 1923.
Church, Archibald. Nervous and Mental Diseases. W.B. Saunders Co., 1923.
Alzheimer Disease
- Characterized by neurofibrillary tangles (aggregates of hyperphosphorylated tau protein) & beta-amyloid plaques
- Generally occurring after age 65
- Hereditary risk factors
- Mutations in the beta amyloid gene
- Epsilon 4 version of apolipoprotein
Diagnosis
- Pathologic diagnosis is the only way to definitively diagnose the condition
- Imaging may be able to rule out other causes of dementia
- Functional imaging studies may be further developed to become diagnostically useful in the future
- CSF studies examining for tau proteins and beta amyloid may become useful as diagnostic tests in the future
Amyloid Plaques & Neurofibrillary Tangles
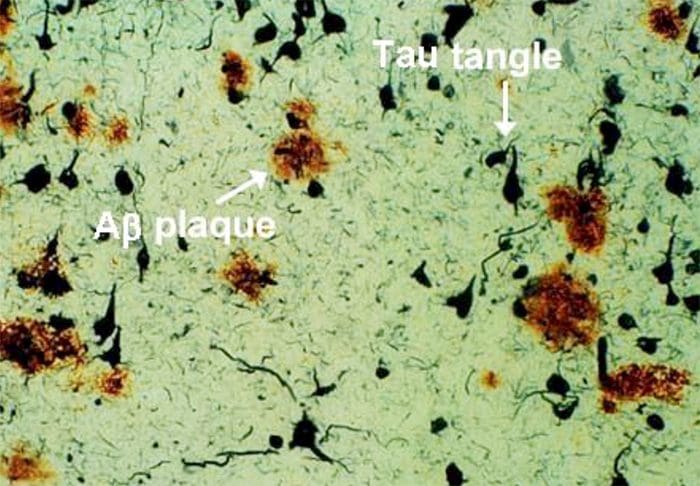 sage.buckinstitute.org/wp-content/uploads/2015/01/plaque-tanglesRNO.jpg
sage.buckinstitute.org/wp-content/uploads/2015/01/plaque-tanglesRNO.jpg
Brain Areas Affected by Alzheimer Disease
-
Hippocampus
- Loss of recent memory
-
Posterior temporo-parietal association area
- Mild anomia & constructional apraxia
-
Nucleus basalis of Meynert (cholinergic neurons)
- Changes in visual perception
Progression
- As more and more cortical areas become involved, the patient will develop more severe cognitive deficits, however paresis, sensory loss, or visual field defects are features.
Treatment Options
-
Medications that inhibit central nervous system acetylcholinesterase
- Donepezil
- Galantamine
- Rivastigmine
-
Aerobic Exercise, 30 minutes daily
-
PT/OT care to maintain activities of daily living
- Antioxidant and anti-inflammatory therapies
- In advanced stages, may require full time, in home care
Vascular Dementia
- Cerebral arteriosclerosis leading to stroke
- Patient will have documented stroke history or signs of prior stroke (spasticity, paresis, pseudobulbar palsies, aphasia)
- May be associated with Alzheimer Disease if due to amyloid angiopathy
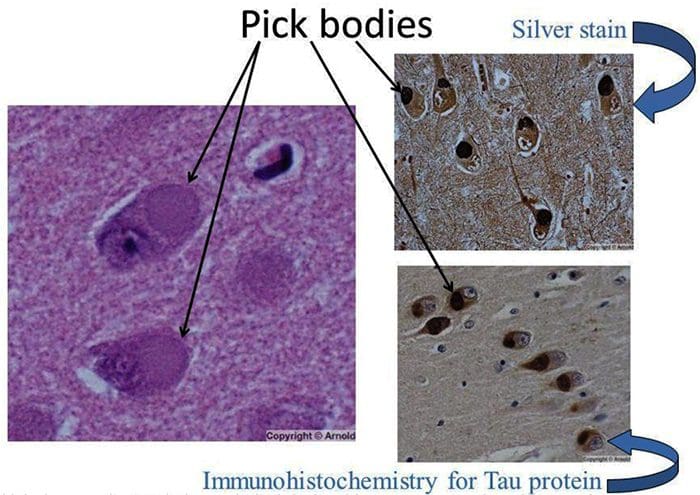
Frontotemporal Dementia (Pick’s Disease)
-
Familial
-
Affects the frontal and temporal lobes
- May be seen on imaging if advanced degeneration in these areas
-
Symptoms
- Apathy
-
Disordered behavior
- Agitation
- Socially inappropriate behavior
- Impulsivity
-
Language difficulties
-
Generally no memory or spatial difficulties
-
Pathology reveals Pick bodies within the neurons
-
Results in death in 2-10 years
Pick Bodies/Cytoplasmic Inclusions
Treatment
-
Antidepressants
- Sertraline
- Citalopram
-
Discontinue medications that can cause memory impairment or confusion
- Sedatives
- Benzodiazepines
-
Exercise
- Lifestyle modification
- Behavioral modification therapy
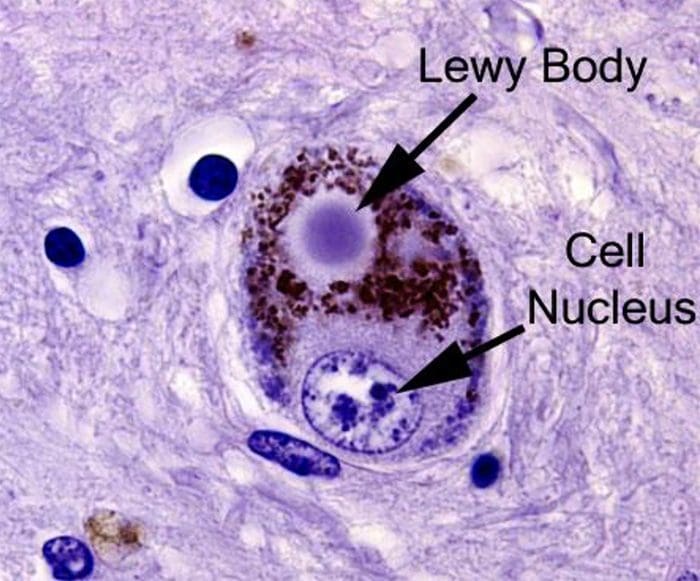
Parkinson Disease
-
May occur at any age, but rare before age 30, and increases prevalence increases in older populations
-
Familial tendency but can also without family history
-
Can be induced by certain environmental factors
- Exposure 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)
- Compounds which produce excessive free radicals
-
Affects substantia nigra pars compacta
- Dopaminergic neurons
-
On pathology, the presence of Lewy Bodies
- Accumulation of alpha-synuclein
Lewy Bodies
 scienceofpd.files.wordpress.com/2017/05/9-lb2.jpg
scienceofpd.files.wordpress.com/2017/05/9-lb2.jpg
Symptoms of Parkinsonism
-
Rigidity (all planes)
- Passive ROM
- Active movement
- May be of cogwheel nature due to tremor symptoms
-
Bradykinesia
- Slowness of movement
- Inability to initiate movement
- Freezing
-
Resting tremor (“pill-rolling”)
- Created by oscillation of opposing muscle groups
-
Postural defects
- Anteriorly flexed (stooped) posture
- Inability to compensate for perturbations, resulting in retropulsion
-
Mask-like facies
-
Mild to moderate dementia
- Later in progression, due to lewy body accumulation
Pathology
-
Deficiency of dopamine in the striatum (caudate and putamen) of the basal ganglia
-
Dopamine normally has the effect of stimulating the direct circuit through the basal ganglia, while inhibiting the indirect pathway
Carbidopa/Levodopa
-
Most common treatment is a combination drug
-
Levodopa
- A dopamine precursor that crosses the blood-brain barrier
-
Carbidopa
- Dopamine decarboxylase inhibitor that does not cross the BBB
- Amino acids will reduce effectiveness (competition) and so medication should be taken away from protein
Prolonged Treatment With Carbidopa/Levodopa
-
The patient’s capacity to store dopamine declines with medication use and therefore the improvements from the medications will last for shorter and shorter periods the longer the medication is used
-
Over time can result in proliferation of dopamine receptors
- Peak-dose dyskinesia
-
Long term use puts stress on the liver
-
Other side effects can include nausea, hypotension and hallucinations
Other Treatment Options
-
Medications
- Anticholinergics
- Dopamine agonists
- Dopanime breakdown inhibitors (Monoamine oxidase or catechol-O-methyl transferase inhibitors)
- High dose glutathione
-
Brain balancing functional neuro-rehab exercises
- Vibration
- Retropulsive stimulation
- Repeated reflex stimulation
- Targeted CMT/OMT
Multiple System Atrophy
-
Symptoms of Parkinson Disease paired with one or more of the following:
- Pyramidal signs (Striatonigral degeneration)
- Autonomic dysfunction (ShyDrager syndrome)
- Cerebellar finding (Olivopontocerebellar atrophy)
-
Generally not responsive to standard Parkinson Disease treatments
Progressive Supranuclear Palsy
-
Fast progressing degeneration involving tau proteins in many areas including the rostral midbrain
-
Symptoms usually start around ages 50-60
-
Gait difficulty
-
Significant dysarthria
-
Voluntary vertical gaze difficulty
-
Retrocollis (dystonic extension of the neck)
-
Severe dysphagia
-
Emotional lability
-
Personality changes
-
Cognitive difficulty
-
Does not respond well to standard PD treatment
Diffuse Lewy Body Disease
- Progressive dementia
- Severe hallucinations and possible paranoid delusions
- Confusion
- Parkinsonian symptoms
Multiple Sclerosis
-
Multiple white matter lesions (plaques of demyelination) in the CNS
- Variable in size
- Well-circumscribed
- Visible on MRI
-
Optic nerve lesions are common
-
Peripheral nerves are not involved
-
Uncommon in children under 10, but usually presents before age 55
-
Viral infection may trigger an inappropriate immune response with antibodies to a common virus-myelin antigen
-
Infectious and immune mechanisms contribute
Types Of MS
-
Primary progressive MS (PPMS)
-
Secondary progressive MS (SPMS)
-
Relapsingremitting multiple sclerasis (RRMS)
- Most common type
- Can develop acutely, spontaneous appear to resolve and return
- Eventually becomes like SPMS
Optic Nerve Involvement
-
In 40% of MS cases
-
Pain with eye movements
-
Visual field defect (central or paracentral scotoma)
-
Funduscopic examination
- May reveal papilledema if the plaque involves the optic disk
- May not appear unusual if plaques are behind the optic disk (retrobulbar neuritis)
Medial Longitudinal Fasciculus Involvement
-
Demyelination of the MLF results in internuclear ophthalmoplegia
- During lateral gaze there is paresis of the medial rectus and nystagmus of the contralateral eye
-
Convergence remains normal
Other Possible MS Symptoms
-
Myelopathy
- Spastic hemiparesis
- Impaired sensory tracts (DC-ML)
- Paresthesias
-
Cerebellar involvement
- Ataxia
- Dysarthria
-
Vestibular system involvement
- Imbalance
- Mild vertigo
- Nystagmus
-
Tic douloureux (trigeminal neuralgia)
-
Lhermitte’s symptom
- Shooting or tingling sensation referred to the trunk and limbs during neck flexion
- Fatigue
- Hot bath often exacerbates symptoms
Differentials To Consider
-
Multiple emboli and vasculitis
- May appear as white matter damage on MRI
-
Central nervous system sarcoidosis
- Can produce reversible optic neuritis and other CNS signs
-
Whipple disease
- Inflammatory lesions
- Usual eye movements
-
Vitamin B12 deficiency
- Dementia
- Spasticity
- Dorsal column
-
Meningovascular syphilis
- Multifocal CNS damage
-
CNS Lyme disease
- Multifocal disease
Differential Diagnosis: Diagnostic Studies
-
Blood tests can help to distinguish
- Complete blood count
- Antinuclear antibodies (ANA)
- Serum test for syphilis (RPR, VDRL, etc.)
- Fluorescent treponemal antibody test
- Lyme titer
- ESR
- Angiotensin converting enzyme level (to r/o sarcoidosis)
Diagnostic Studies Of MS
-
MRI with and without contrast
- 90% of MS cases have detectable MRI findings
-
CSF findings
- Elevation of mononuclear white blood cells
- Oligoclonal IgG bands
-
Increased globulin to albumin ratio
- This is also seen in 90% of MS cases
-
Increased myelin basic protein levels
Prognosis
- Average survival after diagnosis is ~ 15 to 20 year
- Death is usually from superimposed infection and not due to the effects of the disease itself
Sources
Alexander G. Reeves, A. & Swenson, R. Disorders of the Nervous System. Dartmouth, 2004.
Swenson, R. Degenerative Diseases of the Nervous System. 2010.
Post Disclaimer *
Professional Scope of Practice *
The information herein on "Degenerative And Demyelinating Diseases Of The Nervous System" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Our information scope is limited to Chiropractic, musculoskeletal, physical medicines, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somatovisceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and/or functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez, DC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, RN*, CCST, IFMCP*, CIFM*, ATN*
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807, New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Florida
Florida License RN License # RN9617241 (Control No. 3558029)
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Presently Matriculated: ICHS: MSN* FNP (Family Nurse Practitioner Program)
Dr. Alex Jimenez DC, MSACP, RN* CIFM*, IFMCP*, ATN*, CCST
My Digital Business Card